
According to world statistics, about 80% of the adult inhabitants of our vast planet are united by the same health problem: periodically or even constantly, back pain in the lumbar region. Lower back pain is the main symptom of many diseases of the spine and internal organs located in the abdominal cavity. And it is completely useless that most of those who experience discomfort in this area, bypassing the doctor and not understanding the reasons, begin to intensively apply various ointments and other "house lotions". With these methods, you can easily get the opposite of the expected result.
Reasons: to determine, to exclude
The success of any treatment directly depends on the accuracy of the diagnosis, with the elimination of the symptoms felt increases the likelihood of relapse. Subsequently, such treatment can only aggravate the situation. Therefore, first of all, it is necessary to carefully check the condition of all organs, the symptoms of which can be pain in the lumbar region.
Digestive system
Exacerbations of diseases of the digestive system (pancreatitis, ulcers, colitis, cholecystitis, enteritis, appendicitis) often provoke the appearance of pain in the lumbar region.

urinary system
Most often, kidney pain is mistaken for symptoms of diseases of the lumbar spine, as their nature is identical. Diseases of the kidneys and urinary tract of various etiologies are accompanied not only by "recoil" in the lower back, but also by disorders of urination (increased frequency, discomfort, presence of blood in the urine and its turbidity) and an increase in body temperature.
reproductive system
With reproductive organ problems in men and women in the acute stage, the pain often radiates to the lower back, tailbone, or side. The nature of these pains is often a girdle without a pronounced localization.
If a disease of an organ that is not associated with the musculoskeletal system is detected, it is he who is treated, since he is the real cause of the pain syndrome. If, after a thorough examination, no problems with the above organs have been identified, then most likely the problem is with the spine.

Osteochondrosis
The most mobile part of the spine, which accounts for the lion's share of the loads, is the lumbosacral. With a sedentary lifestyle, excessive stress and insufficient nutrient intake in the cartilage tissues of the spine, degenerative-dystrophic changes occur in the intervertebral cartilage in the lumbar region - osteochondrosis.
Symptoms and stages of the disease
The main alarming symptom of osteochondrosis is pain in the lumbar region. At the initial stage, it is localized and directed to the sacrum, its character is pulling (pain). During this period, the processes of destruction affected the nucleus pulposus (its dehydration occurs), as well as the vertebral discs (their standing height decreases). Discomfort is observed with heavy loads, and the pain itself is mild.
After some time, if the problem is ignored and no action is taken, thigh and buttock pulls begin. Due to the narrowing of the intervertebral spaces, the muscles and ligaments "sag" and the spinal column becomes unstable. This leads to loss of sensation and numbness.
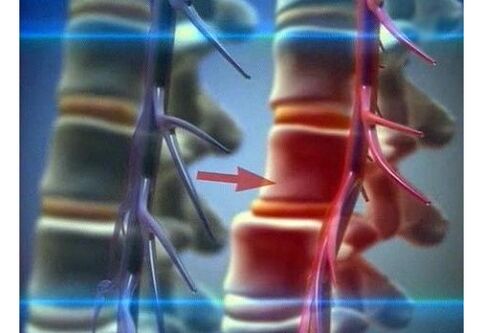
The third stage is characterized by morphological changes in the discs, the spine itself is severely deformed, disc protrusion and prolapse develop. The pain in this phase becomes more intense and prolonged. Each movement brings unbearable pain. It is possible to squeeze areas of the spinal cord, vessels and nerve endings adjacent to the sore spot due to the fact that the fibrous ring protrudes and affects the spinal canal.
The last stage of lumbar osteochondrosis "forces" the body to adapt to the changes that have occurred as a result of the disease in the following way. In order for the supporting and protective functions to be preserved, bone tissue grows in the diseased area. This usually leads to various microtraumas and subsequently to disability.
Comprehensive approach to treatment
Treatment of lumbar osteochondrosis must necessarily be comprehensive, regardless of the stage of development of the disease. With a mild form, the prognosis of treatment is favorable, the deformation processes can be completely blocked and the consequences minimized. At the last stage of the development of the disease, the task of treatment is to eliminate all symptoms and consequences, normalize the nutrition of the spinal tissues, strengthen the muscular corset of the entire back and especially its lower part.
Medicines
To relieve pain in lumbar osteochondrosis, analgesics are used in tablets or injections, the second option is preferable, as it is more effective. To relieve the inflammatory process, anti-inflammatory (non-steroidal) drugs are prescribed. Muscle spasm that occurs simultaneously with pain is eliminated by muscle relaxants. Chondroprotectors are used to restore damaged cartilage tissue.
All these remedies sometimes do not have the desired effect, as the damage prevents the drug from penetrating the site of action.
The block is used to relieve an acute pain attack. Only a specialist should perform it.
A suitable analgesic is injected into the space between the spinous processes with a long needle. After such a procedure, the pain disappears very quickly, but for a while, because there is no therapeutic effect.
Effective use of local complex means: ointments, gels. They have an analgesic, anti-inflammatory and warming effect, many topical preparations contain a chondroprotector. These remedies, when used correctly and combined with massage, are quite effective.
Physiotherapy procedures
In combination with drug treatment for lumbar osteochondrosis, physiotherapeutic procedures are used: balneotherapy, laser and magnetotherapy, treatment with weak currents, light and vibrations. They practically have no side effects and contraindications.
Alternative methods
More and more alternative (non-traditional) methods are used simultaneously with traditional treatment: hirudotherapy, acupuncture, bee stings, manual therapy. These methods give long-awaited relief, but some of them have contraindications, so consultation with the attending physician is required.
In addition to all the above treatment methods, physical therapy helps to overcome the disease. Properly distributed loads of the required intensity will help restore blood circulation to damaged areas, form or strengthen the muscle corset, and thereby unload the spine.
In the treatment of osteochondrosis, it is important to correctly combine the methods of treatment, first of all, attacks of acute pain are relieved, then inflammatory processes, and only when the acute period of the disease has ended, can be non-traditional methods and exercises. .
The Yoga and Pilates complexes have proved to be excellent rehabilitation programs for spinal diseases.
Hernia of the lumbar spine
Against the background of undertreated or neglected osteochondrosis of the lumbar region, a hernia very often develops - a disease in which, due to insufficient physical activity or excessive load, nutrition of the disc tissue occurs, its force decreases and, as a result, disc rupture. The process of destruction can go on for many years and go unnoticed all this time, but with just one unsuccessful movement, the mechanism starts and all the symptoms begin to appear one after another.
General symptoms and course of the disease
Symptoms of a lumbar spine hernia include decreased tendon reflexes, pain of varying intensity, muscle weakness, and numbness in the extremities. Pain with a hernia does not always occur, back pain is possible, gradually spreading in the direction of the pinched nerve.
Distortion of the body is a characteristic sign of a lumbar hernia. This phenomenon occurs involuntarily, as the body needs to find the most comfortable position where pain is minimal. In the severe and rapidly progressive course of the disease, the consequences can be paralysis of the lower limbs (partial or complete). This phenomenon is usually accompanied by disturbances in the functioning of the abdominal organs, especially the intestines and bladder.
Clinical manifestations of a hernia of the lumbosacral zone are expressed in a constant increase in pain and their intensification during specific physical exertion (weight lifting, bending, sharp sharp muscle tension, cough), dull aching pain with localization in a place that not go away, the direction of pain in the buttock or leg, or numbness in that area.
Diagnosis of a hernia of the lumbar spine
It is difficult to diagnose a hernia visually or by the symptoms described by the patient alone. To more accurately determine the presence of the disease, several methods are used that will help to accurately determine the location of the disease. Computed tomography, nuclear magnetism and radiography - thanks to these methods, the doctor will be able to visually determine the position of the pathologically altered vertebra and see the deformed disc.
To determine the severity of the disease and its consequences, doctors use several tests: straightened leg lift, tendon reflexes, sensitivity (reaction) of the leg at all levels (from toes to hip joint) to different types of stimuli - pain, vibration and temperature.
Methods of treatment
Depending on the severity and condition of the patient, different methods of hernia treatment are used. In case of exacerbation, first of all, it is necessary to immediately limit motor activity until bed rest and relieve pain with medication. After 5-7 days, when the acute period has ended and the pain has subsided, drug treatment is supplemented with other restorative procedures (massage, physiotherapy, physical education).
Medical and conservative treatment of lumbar hernia is the same as for osteochondrosis.
Surgery
In case of a severe course of the disease and the presence of many serious consequences, surgical treatment is recommended.
Indications for surgery:
- seizure of a hernia - a part of the disc damaged by a hernia enters the spinal canal;
- dysfunction of all or one pelvic organ;
- patency in the spinal canal is impaired (determined by MRI);
- lack of results when using a medical and conservative method of treatment for three or more months;
- inflammation of the sciatic nerve.
Surgical treatment of a hernia is now being performed with the help of minimal and minimally invasive endoscopic operations.
The laser reconstruction method consists of evaporating the fluid from the protruding nucleus pulposus using a laser. Thanks to this, the nerve root is "released", ie its compression is eliminated. But this type of surgery has a number of contraindications, these are early operations on the spine, spondylolisthesis, spondyloarthritis, impaired patency of the spinal canal (stenosis) and protrusion of the nucleus pulposus in the canal.
To remove the damaged part of the intervertebral disc, the percutaneous discectomy method is used. Evaporation and removal of damaged tissue is done with a needle inserted through the skin.
In the event that it is impossible to restore the damaged disc in any way, starting with the dressing and ending with a minimally invasive operation, or all the methods used do not bring any results, the deformed disc is replaced with a prosthesis.
Preventive measures
In order to prevent the progression of the disease, special exercises are prescribed. Exercise complexes should be developed by a specialist individually for each patient and should contain exercises for muscle stretching, tension and light aerobic exercise.
With a hernia of the lumbar spine, doctors recommend wearing a special fastening belt. Outwardly it resembles a capsule, its width is about 30 cm, it is attached to the body with Velcro and has different degrees of rigidity.

This product is necessary to evenly distribute the load (from the diseased to the healthy area) and relieve stress (discharge). Damaged segments of the spine with constant use of the belt are corrected and returned to their anatomical position.
Low back pain with radicular syndrome
Against the background of osteochondrosis and hernia of the lumbar spine, as a result, low back pain develops: lumbar back pain (acute paroxysmal pain). This is the "simplest" scenario. Since hernias and osteochondrosis are characterized by deformation and frequent prolapse of the damaged disc and displacement of the spine, there is a violation of nearby nerve roots, called radicular syndrome.
It is amplified by the violation of the veins, which causes tissue (soft) edema and congestion. Symptoms of low back pain with radicular syndrome are similar to symptoms of a lumbar hernia (sharp stabbing pains radiating downward, loss of sensation and impaired reflexes), and since this is a consequence, the cause should initially be treated with a integrated approach, otherwise disability threatens.
Sciatica
Another consequence of hernia and osteochondrosis is inflammation of the sciatic nerve - sciatica and the pain radiating to the leg or buttock that accompanies it. Despite the ability to clearly define the "sore" spot, the reason lies in the spine.
Sciatica is not an independent disease, this term refers to a number of symptoms that accompany certain diseases of the spine. The pain sensations can be different, in some cases it is just a slight discomfort when staying in the same not very comfortable position for a long time, and sometimes the pain leads to loss of consciousness, and analgesics in this case do not help.
For effective treatment, it is not enough to diagnose sciatica or low back pain, in any case it is necessary to conduct a comprehensive comprehensive examination by various specialists and accurately identify the cause, because this is precisely the provoking factor. With the elimination of only some of the symptoms, the likelihood of the progression of the underlying disease and the appearance of many complications increases. Health-conscious attitude, early recognition of problems and prompt treatment are the key to good health.

















